Connect With Us
Items filtered by date: January 2022
How to Avoid Falling in Your Own Home
Once you reach the age of 65, you are much more likely to fall and suffer a serious injury. With most people in this age group taking a tumble in their own home, it makes sense to keep your own dwelling as safe as possible to avoid “falling” into this category yourself. First, make sure there is an adequate amount of lighting throughout your home. You’ll also want to remove tripping hazards such as clutter, loose rugs, unsecured wires, and unstable furniture. Fix any uneven surfaces in and around your home. Install grab bars in the shower and next to the commode, as well as non-slip mats in the bathroom and kitchen. Keep stairs clear of clutter, make sure the handrails on your stairs are secure and that you use them, and always take your time walking up and down the stairs. Be mindful of your steps and try not to rush around. It is also important to identify any medically related risk factors such as gait abnormalities or other foot conditions that may affect your balance and sure-footedness. Make an appointment with a podiatrist who can offer advice on proper footwear, and fix any foot or ankle conditions that may be compromising your foot health.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Ali Davis, DPM from The Foot Clinic. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Overland Park, KS . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton’s Neuroma in Runners and Others
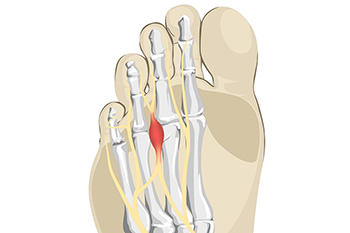 Many runners develop a condition known as Morton’s neuroma which is a thickening of a nerve in the foot. It usually affects the large nerve between the third and fourth toe, which is more susceptible to pressure, irritation and injury, and results in painful inflammation. Runners and people playing sports that involve pressure on the ball of the foot are more apt to develop this condition. Also, women wearing high heels, with a lack of room in the toe box and improper cushioning are susceptible. People with flat feet, high arches, bunions or hammertoes are also at risk. Morton’s neuroma is thought to be a progressive ailment, and for that reason diagnosis is often delayed until the condition becomes more severe. At some point, the symptoms become more painful and frequent and last longer. Many people complain of having a pebble in their shoe or feel like their sock is bunched up. It is suggested that you consult with a podiatrist at the earliest onset of such symptoms for a diagnosis and treatment plan.
Many runners develop a condition known as Morton’s neuroma which is a thickening of a nerve in the foot. It usually affects the large nerve between the third and fourth toe, which is more susceptible to pressure, irritation and injury, and results in painful inflammation. Runners and people playing sports that involve pressure on the ball of the foot are more apt to develop this condition. Also, women wearing high heels, with a lack of room in the toe box and improper cushioning are susceptible. People with flat feet, high arches, bunions or hammertoes are also at risk. Morton’s neuroma is thought to be a progressive ailment, and for that reason diagnosis is often delayed until the condition becomes more severe. At some point, the symptoms become more painful and frequent and last longer. Many people complain of having a pebble in their shoe or feel like their sock is bunched up. It is suggested that you consult with a podiatrist at the earliest onset of such symptoms for a diagnosis and treatment plan.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Ali Davis, DPM of The Foot Clinic. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Overland Park, KS . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Warts Can Be Treated!
What Happens During an ABI Test?
An Ankle-Brachial Index (ABI) test is a fast, relatively painless, and non-invasive screening measure used to detect a person’s risk of having peripheral artery disease or other problems with blood flow in the lower limbs. During an ABI test, your doctor will use a blood pressure cuff to measure the blood pressure at various locations along your calves, feet, and toes, as well as at your upper arms. These measures are then used to calculate a ratio that corresponds to your risk of having impaired circulation. You may feel slight, momentary discomfort while your blood pressure is taken, but this test has no other risks or complications associated with it. For more information about ABI tests, please consult with a podiatrist.
Vascular testing plays an important part in diagnosing disease like peripheral artery disease. If you have symptoms of peripheral artery disease, or diabetes, consult with Ali Davis, DPM from The Foot Clinic. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Vascular Testing?
Vascular testing checks for how well blood circulation is in the veins and arteries. This is most often done to determine and treat a patient for peripheral artery disease (PAD), stroke, and aneurysms. Podiatrists utilize vascular testing when a patient has symptoms of PAD or if they believe they might. If a patient has diabetes, a podiatrist may determine a vascular test to be prudent to check for poor blood circulation.
How Is it Conducted?
Most forms of vascular testing are non-invasive. Podiatrists will first conduct a visual inspection for any wounds, discoloration, and any abnormal signs prior to a vascular test.
The most common tests include:
- Ankle-Brachial Index (ABI) examination
- Doppler examination
- Pedal pulses
These tests are safe, painless, and easy to do. Once finished, the podiatrist can then provide a diagnosis and the best course for treatment.
If you have any questions, please feel free to contact our office located in Overland Park, KS . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Can I Do When a Wound Doesn’t Heal?
If you have a wound for more than 8 weeks and it still hasn’t healed, it may be considered to be chronic. Such an occurrence could be caused by poor circulation, diabetes, or a weak immune system. Open wounds on the lower leg are known as venous leg ulcers. These kinds of wounds may be medically treated by removing the dead or inflamed tissue, known as debridement. The wound itself can then be cleaned by a high-pressure water jet. A local anesthetic may be used as this treatment is said to be painful. Afterward, the wound should be covered with gauze or a similar dressing to keep it from becoming infected. Compression stockings may be prescribed to increase circulation. For more information on chronic wounds in the feet or ankle area, please consult a podiatrist.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Ali Davis, DPM from The Foot Clinic. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Overland Park, KS . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019